by Dr.Harald Wiesendanger– Klartext
What the mainstream media is hiding
One in five women over 50 already have osteoporosis – their bone density has decreased dangerously, and there is a risk of fractures. However, conventional treatment only reliably benefits pharmaceutical companies, doctors’ practices, and clinics, and it often worsens the situation of those affected. Simple measures could restore and maintain bone health – much cheaper and free of side effects.
Ottilie, the average person, has a very harmonious marriage with the well-known Joe Average, on equal terms, closely connected by many things in common. Among other things, both are very interested in health issues. Because they pick up every free pharmacy brochure and always study the medical page of their local newspaper, they believe they are well informed.
That is why Ottilie, 53, cannot possibly remain unmoved by what she recently read: one in five women over 50 has osteoporosis. Most of them have no idea about it. Because they have no symptoms, their bones become increasingly porous imperceptibly until one day they break – and never heal. Alongside arthritis, cardiovascular disease, diabetes, dementia, and loss of vision and hearing, Ottilie learns that osteoporosis is one of the most common causes of disability among senior citizens: after an osteoporotic fracture, one in four sufferers can no longer look after themselves and becomes in need of care; According to the German Osteology Association (DVO), one in five people dies in the first year after a severe hip fracture.
Because such prospects worry her, Ottilie gets her family doctor to refer her to an orthopedic specialist. “It’s good that you’ve finally come,” he says, “at your age, it’s high time to measure your bone density.” The results show at least a precursor to osteoporosis: osteopenia. The doctor prescribes Ottilie a calcium supplement and vitamin D – “it helps to absorb calcium from the intestines and incorporate it into the bones.” He also advises her to eat more dairy products. She is to return for a check-up in a year.
With this first measurement, Ottilie begins a typical patient career, the reasons for which she has no idea until the very end.
Shortly after she starts taking calcium, she constantly has digestion problems. Bloating, constipation, and diarrhea are part of her everyday life. She reads somewhere that this could be due to lactose intolerance. So, she avoids dairy products and eats more kale, broccoli, and spinach. Or is she intolerant to gluten? From now on, she will avoid baked goods made from wheat, rye, and barley. Or does she have difficulty digesting fructose? As a precaution, she avoids fruit with a high fructose content.
But the symptoms remain. Could it be stomach ulcers? Gallstones? Pancreatitis? Crohn’s disease? Or ulcerative colitis? Ottilie has checked all of these things out by a doctor, but nothing has been found.
The next bone density measurement is due by the time she has this cleared up. Unfortunately, it does not give her any reason to give the all-clear; on the contrary, the value has worsened and is now indicating the onset of osteoporosis.
Of course, the orthopedist has some advice: “Apparently, calcium is not enough for you. I will now prescribe you a medication that you will take in addition from now on, once a week – a so-called bisphosphonate. It inhibits bone loss. Reliable. And well tolerated.” It is called “Fosamax.” “We’ll see each other again in a year.”
The next reunion, however, takes place just a few weeks later. Ottilie is suffering from new symptoms: constant heartburn, nausea, stomachache, and pain in muscles, bones, and joints. “It may be due to your osteoporosis medication,” the family doctor suspects and sends her to the orthopedist again. “It can happen that you don’t tolerate a certain medication very well,” explains the specialist. He gives Ottilie a prescription for “Actonel.”
But her symptoms don’t change. Neither do “Bonviva” and “Aclasta.”
What else can Ottilie do but bravely endure her symptoms? “Not breaking any bones is more important.” She is prescribed a proton pump inhibitor for her heartburn. Her digestive problems then become worse. She often feels dizzy. Her head and stomach ache even more often.
For twenty years, she has been taking drugs to prevent bone loss, strictly following the instructions in the package insert. And she continues to have her bone density measured regularly. She is pleased to learn that the value is gradually improving. This makes it easier for her to endure the persistent side effects of the pill therapy. She can manage her pain quite well with ibuprofen – but in the long term, it causes her to develop gastritis and duodenal ulcers.
At least her menopausal symptoms have improved a little since her gynecologist prescribed estrogens. “Studies show that they also strengthen her bones,” he says.
Ottilie was 73 when she tripped over the edge of a carpet, fell awkwardly – and suffered a complicated fracture of the hip joint. It did not heal.
The pensioner never recovered from this. She remained confined to a wheelchair for the last decade of her life – and terminally ill because hormone replacement therapy had led to breast cancer. Fed with that notorious, not necessarily bone-friendly type of culinary euthanasia for which Germany’s old people’s homes are notorious, she closed her tear-stained eyes forever in a nursing home full of metastases – a few months after her Otto. He had died of a heart attack shortly after the second corona “booster.”

Fallen into the pharmaceutical trap
Ottilie is fictitious; her medical history is not at all. Year after year, millions upon millions of supposed “high-risk patients” allow themselves to be scared to death of brittle bones; after that, they unknowingly, in a blind trust in the expertise of their orthopedists, surrender themselves to a perverse medical system that produces disease instead of curing it – that is how it thrives. Far too many people pay a high price for their gullibility.
The story of this scandal begins in 1992, with the World Health Organization as the shameful main actor. In the early 1990s, the WHO arbitrarily concocted today’s definitions of osteopenia (1992) (1) and osteoporosis (1994) (2). From then on, doctors understood this to mean skeletal diseases that are not characterized by specific complaints. Still, by a measured value: in these cases, the bone mineral density (BMD) in the hip, measured in g/cm2 or g/cm3, is 1 or 2.5 standard deviations below the peak bone mass of an average, approximately 30-year-old Caucasian (3) woman, as determined using an X-ray device known as dual-energy X-ray absorptiometry (DXA or DEXA). A “standard deviation” is nothing more than a statistical calculation that expresses the extent to which a group within a population deviates from the mean: for example, in terms of height, weight, muscle mass, cholesterol level, intelligence – or in the ratio of mineralized bone substance, which consists mainly of calcium and phosphate crystals, to a particular bone volume.
This is the basis for the “T-score” orthopedists derive from BMD measurements for their patients. It is expressed in standard deviations (SD). The WHO has set the following limits for their interpretation:
– T-score ≥ -1.0 SD: Normal bone density
– T-score between -1.0 and -2.5 SD: Osteopenia (precursor to osteoporosis)
– T-score ≤ -2.5 SD: Osteoporosis.
This completely arbitrary terminology has serious consequences for people with a skeleton:
– For statistical reasons, they can suffer from a disease that requires treatment without experiencing the slightest symptoms.
– This symptom-free disease worsens unnoticed and with inexorable necessity the longer they reach their 30th birthday. After all, it is part of the natural aging process for every person that bone mineral density gradually decreases. According to the WHO definition, by the age of 25, 15% of the population already “suffer” from osteopenia without experiencing the slightest pain; among 50-year-olds, the figure is already 33%. And 60% of 65-year-olds have to accept that they either suffer from osteopenia (40%) or already have osteoporosis (20%).
Bone density changes with advancing age depending on gender
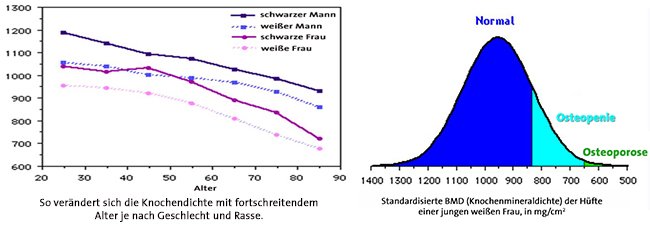

But how logical is it to use the standard bone density of a young adult as a benchmark for all of us, regardless of age? Wouldn’t it be more logical to use the “Z-score” that compares our BMD with that of our age group, gender, and ethnicity? As soon as you do that, a huge “burden” of disease suddenly disappears into thin air. According to a study published in the Journal of Clinical Densitometry in 2009, 30% to 39% of subjects diagnosed with osteoporosis using DXA technology would be classified as either normal or merely “osteopenic” if the Z-score were used instead of the T-score.
Suppose you investigate the conflicts of interest within the expert panel whose recommendations the WHO bases its terminological acrobatics on. In that case, you will suspect that this intention has less to do with promoting health than with supporting business models based on the loss of health. To this end, a normal aging process is pathologized. With a sleight of hand, it is transformed into a disease that requires treatment and can be targeted with expensive diagnostics in order to justify the use of costly medication. “We have medicalized a non-problem,” admits Dr. Michael McClung, director of the Oregon Osteoporosis Center. (4)
The tried and tested use of mathematical and clinical jargon, coupled with academic arrogance, prevents confused laypeople from seeing through the game.
The semantic charade served economic purposes. Because, in the tried and tested manner, it paved the way for abnormal “preventive medicine” – not in the sense of measures that reduce the risk of disease, but mass preventive examinations to detect diseases at great expense. Such lucrative screenings soon become the norm. (A DEXA scan usually costs between 50 and 150 euros – and, of course, has to be carried out as often as possible so that the DEXA device, which costs 23,000 to over 35,000 euros, pays for itself.) The lower the threshold for pathology, the sooner the alarm sounds that it has been exceeded, and the more justified it seems to sell medical products and services tailored to it. The lower the “safe” blood pressure and the “safe” cholesterol level, the more blood pressure-lowering drugs and statins can be prescribed. The WHO definitions of osteopenia and osteoporosis make it possible to play the same infamous game with bone density.
The price is hot; the market is enormous: In Germany, 6% of the population is said to be affected by osteoporosis (5), an estimated 6.5 to 8 million; four-fifths of these are women after menopause. “At the age of 70, osteoporosis is a widespread disease,” says internist Johannes Pfeilschifter, who has been coordinating the development of the osteoporosis guideline for twenty years, a guide to diagnosis and therapy. Around 200 million people worldwide are probably affected, Which means that the business is a multi-billion dollar business.
The interior of a bone with osteoid collagen fibers and stored calcium rendered by Microsoft AI big image creator
Pharmaceutical treatment for osteoporosis:
more harm than good
But how many osteoporosis patients ever hear from their doctors how fatal a fabulous BMD can be? Several studies have now shown that an above-average bone density increases the risk of breast cancer in middle-aged and elderly women by 200% to 300%. (6)
Calcium supplements in megadoses, which countless women take as a precaution, increase the risk of a heart attack by 24 to 27%, as shown by two meta-analyses published in the Lancet in 2011 (7), and by 86%, as shown by a more recent meta-analysis published in the journal Heart. The more than 1,200 milligrams of pure calcium that the US Bone Health and Osteoporosis Foundation (BHOF) recommends that women over 50 take to “protect their bones” could also cause coronary artery spasms, arteriosclerosis, and kidney stones in millions of women. (In reality, even more than 500 mg can be problematic.) It is unlikely that the influential organization will change its mind any time soon: its sponsors include the manufacturers of the calcium supplements Citrical and Oscal.
Why does it make little sense to simply consume plenty of calcium? Even if some textbooks lump the two together, osteoporosis is not the same as osteomalacia, a disorder in which minerals dissolve from the bone due to a lack of calcium, causing it to soften. In osteoporosis, the framework of the bone substance is lost: the osteoid, a matrix that consists mainly of collagen fibers. It is formed by specialized cells, the osteoblasts, which develop from stem cells in the bone marrow. In doing so, they release osteonectin, a hormone that causes calcium to bind to the fibers and store itself in their soft network to strengthen it. If this matrix thins out with advancing age, more calcium is of little use – because there is no structure in which it can store itself. You might as well dump cement on a building site without first putting up formwork.
What about the increasingly frequently prescribed Bisphosphonates: active substances that switch off or kill osteoclasts – the cells that break down bone substance? In fact, they ensure that bone density increases because the balance of bone production shifts in favor of bone formation. But the bones that form are much more brittle and inflexible. This explains why bisphosphonates paradoxically increase the risk of bone fractures – especially unusual hip fractures – which subsequently heal more poorly. If taken over a long period of time, they can promote the formation of bone fissures – microfractures – i.e., fine cracks or gaps in the bone, which massively inhibits its ability to heal. Significantly, of 70 patients who were admitted to Presbyterian Hospital/Weill Cornell Medical Center in New York between 2002 and 2007 for femur fractures, 25 were taking the bisphosphonate Fosamax. Of 20 who suffered a so-called stress fracture (“fatigue fracture”) during the five-year observation period – a special type of bone fracture caused by repeated overloading – 19 had taken Fosamax.
This devastating “success report” from 2007 was confirmed four years later by a Swedish study of more than 12,700 women over 55: Of 59 who suffered femur fractures, 78% had taken bisphosphonates. “The connection between bisphosphonates and the fractures is so striking that it can be confirmed as a causal connection,” explains the study leader.
In addition, this type of medication has many nasty side effects. The most common include: stomach irritation; inflammation of the esophagus, even cancer; severe bone, muscle, and joint pain throughout the body; death of bone tissue in the jaw; flu-like symptoms; atrial fibrillation; declining kidney function; inflammation of the eyes; and hypocalcemia – too low a calcium level in the blood, which can cause muscle cramps and numbness in the limbs, and in severe cases even epileptic seizures.
But how many patients, no matter how severe the side effects, ever get the idea to question the pharmaceutical approach fundamentally? If they don’t like a certain product, most people will go for the next one that the doctor recommends – he should know, right? (I show how conventional doctors usually acquire their specialist knowledge in the article series “Trained Demigods.”)
Often, those affected are prescribed Hormones for what appears to be a good reason: estrogens play a crucial role in bone metabolism. If there is a lack of them, bone-degrading cells (osteoclasts) live longer, while the lifespan of bone-building cells (osteoblasts) is shortened; this leads to increased bone loss during menopause. Studies have actually shown that with several years of hormone replacement therapy, bone fractures are 25% less common, and the risk of hip and vertebral fractures is even reduced by a third. (8) However, estrogen supplements increase the risk of breast, ovarian, and endometrial cancer; heart disease; life-threatening thromboembolism – blockages of blood vessels because a blood clot travels further within the vascular system -; gallbladder disease; incontinence, strokes, and dementia. (9)
The most important hormone that gives bones elasticity and stimulates osteoblasts is progesterone. Like estrogen, it decreases with age, especially after menopause. If supplemented appropriately – which, unlike estrogen, is almost always safe – progesterone is very effective in preventing bone fractures. Depression, migraines, severe allergic reactions with a drop in blood pressure, and cardiac arrhythmias occur very rarely. But the risk exists.
Will a new class of drugs provide relief: Selective Estrogen Receptor Modulators, or SERMs for short, such as “raloxifene” and “bazedoxifene”? These influence estrogen receptors selectively: in some tissues, e.g., bones, they have estrogen-like effects; in others, e.g., the breast, they have an anti-estrogenic effect. SERMs thus enable more differentiated treatment than with classic hormone replacement therapy. At first glance, they seem to elegantly avoid the dangers of these while at the same time preserving their benefits. They increase bone density, prevent breast cancer, and relieve menopausal symptoms. (10)
Unfortunately, SERMs do not eliminate serious risks: there is a risk of venous and pulmonary thrombosis, strokes, and gallbladder disease. Headaches and migraines, flu-like symptoms, gastrointestinal complaints, skin rashes, calf cramps, edema, and high blood pressure often occur.
So is the way clear for the next pharmaceutical “innovation”: RANKL inhibitors such as “denosumab”? Such active ingredients, tailor-made monoclonal antibodies, bind and neutralize RANKL, a protein that plays a key role in osteoclasts forming, functioning, and surviving. They interrupt the interaction between RANKL and its receptor, located on the osteoclast precursor cells’ surface. This prevents new osteoclasts from forming. (11)
If you read the package insert carefully, however, your hair will stand on end once again: infections of the urinary tract and upper respiratory tract are common; allergic skin reactions; Pain in the muscles and skeleton. There is a risk of hypocalcemia. Immune deficiency, impaired wound healing, inflammation, and jaw necrosis can also occur. Atypical fractures of the femur and multiple vertebral fractures can occur – the very catastrophes that the drug is supposed to protect against. (12)
But what does the healthcare industry care about any collateral damage from their products as long as the returns satisfy investors? Global sales of osteoporosis drugs currently amount to 8 to 11 billion US dollars annually (13), with annual growth rates of 3 to 4% – to the satisfaction of market leaders Eli Lilly, Hoffmann-La Roche, Pfizer, Merck, and Amgen.
Market shares of osteoporosis drugs worldwide (2018)

Ensuring bone health would be so easy
From the age of 30, up to one percent of bone mass is lost every year. After menopause, women lose up to 20% of this within 5 to 7 years. Isn’t it advisable to counteract this process as early as possible before it manifests itself in the worst possible way in the event of a fall? Why just watch as bones become more and more brittle until one day they break?
The rhetorical question would hit the nail on the head if what it assumes were true: that the risk of bone fracture depends exclusively or at least mainly on mineral density. But that is by no means the case. BMD and bone strength are partially correlated – but they are not equivalent. Density may be a reliable indicator of how resistant a bone is to breaking when a static weight is applied to it – but it says little about how stable it remains under tension or stretching. “In some cases, higher bone density even indicates that the bone is weaker,” explains Sayer Ji, founder of the medical information service Greenmedinfo.com: “Glass, for example, has a high density and compressive strength, but is extremely brittle, which is why it breaks easily when it falls to the ground. Wood, on the other hand, which is naturally closer to the human bone than glass or stone, has a lower density compared to these materials but is also extremely strong and can bend and stretch to withstand exactly the same forces that the bone is exposed to in a fall. Or take a spider’s web. It has infinitely greater strength and practically no density. Given these facts, high bone density – and therefore no osteoporosis – can actually increase the risk of fracture in a real scenario such as a fall.” How real this risk is is experienced by all too many osteoporosis patients who, like Ottilie, have dutifully taken the prescribed medication for years (decades) – and still suffer serious bone fractures.
“The most important thing,” emphasizes an American doctor who, for good reason, hides behind the pseudonym “A Midwestern Doctor” – “is not bone density, but the elasticity and mobility of bones. When healthy bones are subjected to stress, they bend to compensate for the stress and then return to their original shape, while a brittle bone breaks as soon as it begins to bend.”
The WHO definitions, therefore, tempt people to underestimate crucial aspects of bone quality and the actual risk of fracture. In doing so, they divert attention and resources away from less profitable but more effective approaches: changing lifestyle, improving nutrition, addressing underlying health problems.
The be-all and end-all: healthy lifestyle habits
The safer you can walk, the lower the risk of having a serious fall and breaking a bone; this, in turn, depends crucially on how much you move. We sit too much. The research is clear: regular physical exercise promotes a healthy bone structure and makes fractures less likely. In a US study, women who spent most of their day sitting lost 2.26% of their bone mass after menopause within a year, while those who did a strength training program instead saw an increase of 1.17%.
Why is regular physical activity so crucial for osteoporosis? Only physical exertion stimulates osteoblasts, cells that are responsible for building and regenerating bone substance. They detect minor defects in the bone tissue and repair them.
Through targeted exertion, bones gain stability because the fine bone beams – trabeculae – strengthen and network, following Wolff’s law (14), according to which bones adapt to stress.
Exercise also strengthens muscles. Strong muscles stabilize the body. They protect against fractures by improving balance, coordination, and sure-footedness. Those who can keep their balance, avoid obstacles, and support themselves when falling are more likely to avoid fatal falls.
A health system that was actually interested in preventing and treating osteoporosis effectively, cheaply, and without side effects would create the most attractive incentives possible for couch potatoes, both healthy and affected, to get up off their butts: for regular strength training, for balance exercises, for endurance sports such as brisk walking, Nordic walking or slow jogging. But every little dance, every hop, every climb up the stairs has a preventative effect.
Why in the fresh air? There, we are exposed to sunlight, which also increases bone density because it stimulates the body’s own production of vitamin D, which is essential for calcium absorption.
Our risk of osteoporosis decreases further as soon as we say goodbye to certain lifestyle habits. Too much alcohol impairs calcium absorption, which disrupts bone formation. Excessive caffeine increases calcium excretion through urine, which can also have a negative impact on bone density. Smoking impairs blood circulation and the function of bone-building cells (osteoblasts) and calcium absorption. E-cigarettes appear to be even more harmful than conventional cigarettes.
What about obesity? For a long time, the prevailing opinion was that a higher body weight protects the bones because it places greater mechanical stress on them, which benefits bone density. We now know more: obesity, especially when it is accompanied by a high proportion of visceral fat – around the internal organs – promotes chronic low-grade inflammation in the body. This can increase the activity of osteoclasts – the bone-degrading cells – and disrupt bone metabolism. Leptin and adiponectin – hormones secreted by fatty tissue – promote the breakdown of bone tissue in high concentrations. In addition, fatty tissue can accumulate in the bone marrow if you are severely overweight; it impairs the normal function of the bone-forming cells (osteoblasts) and weakens bone structure.
Severe underweight and frequent diets also have a negative effect on bone metabolism.
Eating away the risk
“Let food be your medicine,” the Greek physician Hippocrates is said to have taught four centuries before Christ. He was also spot on with regard to our bone health. The risk of osteoporosis depends on our diet. Eating a lot of fast food, soft drinks, and sweets increases it, as does too much animal protein and artificial phosphates, such as those found in sausage and many convenience foods. (Phosphate additives in processed foods disrupt the ideal ratio of calcium to phosphorus in our diet.) If you eat unhealthily, you don’t consume enough calcium, vitamin D, and other essential nutrients for bone health. Too much salt promotes calcium excretion.
What does a bone-friendly diet look like? It should be Mediterranean – with a high proportion of plant-based foods, whole grain products, olive oil as the primary source of fat, little red meat, moderate amounts of fish, poultry, and dairy products, with beans, nuts, and other legumes. This is supported by a study presented in March 2018 at the annual meeting of the Endocrine Society in Chicago. The diet, bone density, body fat percentage, and skeletal muscle mass of 103 women, an average age of 55 and thus in menopause, were analyzed. It was found that the better the participants followed the rules of the Mediterranean diet, the higher their bone density.
Mediterranean Vegan Recipes: The Most Popular And Delicious
Start your day with Millet; it helps prevent acidification
In order to provide the body with sufficient calcium, pharmaceutical products are generally not required. Many foods provide it in abundance: above all, soybeans, kale, broccoli, dried figs and broad beans, linseed, sesame, hazelnuts and almonds, milk and whey drinks from curd production, some types of cheese, calcium-rich mineral water.
An unbalanced acid-base balance, especially chronic hyperacidity, damages bone health and increases the risk of osteoporosis. In the case of hyperacidity, the body tries to keep the pH value of the blood in the neutral range. To neutralize excess acids, it uses alkaline minerals, mainly calcium from the bones – which leads to the bone substance being broken down. This speaks in favor of a diet rich in alkaline foods. These include many fruits, vegetables, nuts, seeds, herbs, and spices.
See> What Is A Basic Diet Or Alkaline Diet and Why An Alkaline Diet,
See also >Why Alkaline Vegan Recipes Are Good For Your Health
How To Make A Alkaline Diet Benefit You – Why You Need These Amazing Greens In Your Alkaline Diet – Are You Acidic? Symptoms That Show And What Can Help
Why Alkaline Vegan Recipes Are Good For Your Health
Chronic inflammation also promotes osteoporosis, so it must be recognized and remedied. This is because it leads to increased production of cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-1 (IL-1) and interleukin-6 (IL-6). These stimulate the activity of osteoclasts, which leads to increased bone breakdown. An anti-inflammatory diet, which essentially corresponds to the Mediterranean diet, therefore reduces the risk of osteoporosis: one with plenty of fruits, vegetables, sprouts and salads, whole grain products, nuts, seeds, legumes, fish, or other sources of omega-3 fatty acids.
How Food Can Help You Avoid Inflammatory Conditions
The benefits are impressively demonstrated by data from the Women’s Health Initiative (WIH) Study, the most extensive health study of postmenopausal women ever conducted in the USA. In over 160,000 participants with an average age of 63 who had never suffered a hip fracture before the start of the study, hip fractures occurred more frequently over the six-year observation period the more inflammatory components their diet contained; their risk increased by 50%. Bone density values were also available for 10,290 of these women; these decreased significantly less when they ate an anti-inflammatory diet. (15)
Because bones are made of minerals, bone strength depends on our intake of them through food: in addition to calcium, magnesium, phosphorus – after calcium, the most abundant mineral in the human body (16) -, potassium and silicon (17) as well as trace elements such as zinc (18), boron (19) and copper. Unfortunately, there is an increasing lack of these. Industrial agriculture has chronically depleted farmland of essential micronutrients and minerals. Mineral-rich components of food are removed during processing, e.g., when refining whole grains. Glyphosate, the ubiquitous pesticide, acts as a chelating agent, binding essential minerals in the soil, especially the +2 cations such as magnesium – thus preventing them from entering our bodies.
Why Is Magnesium Important To Keep You Healthy? – Magnesium – Rich Food That Can Help To Keep You Fit – Vitamin B12 Myths
Vitamins also play an active role in bone formation, in addition to D, especially folic acid (B9), B12, C, and K. Only with vitamin K can the protein osteocalcin, which binds calcium, be formed in the bones; if there is a lack of this, the risk of osteoporotic bone fractures increases considerably, as shown in a 1999 study with over 72,000 participants. (However, vitamin K and D must be in a balanced ratio. If there is a lack of vitamin K, a simultaneous excess of vitamin D increases the risk of osteoporosis further.) Particularly rich sources of vitamin K are green leafy vegetables and herbs, especially kale, but also broccoli, cauliflower, Brussels sprouts, spinach, purslane, chives, and parsley. Alternatively, a grass powder is suitable – depending on your taste preferences, made from wheat, kamut, barley, or spelt grass, stirred in water, or your own favorite juice.
Isoflavones – plant substances with potent antioxidant, anti-inflammatory, and hormone-regulating effects – can also help protect against osteoporosis. They are abundant in soy and medicinal plants (20), such as skullcap, horsetail, nettle, red clover, chasteberry, and black cohosh. Linseed oil also seems to protect and strengthen our bones.
But if all of this still doesn’t help? Then homeopathy and Schuessler salts, even acupuncture, are definitely worth a try. There are plenty of encouraging reports. And even if such unconventional approaches are less effective than hoped, patients are at least spared the nasty side effects of pharmaceutical drugs.
And what if the osteoporosis is “secondary,” i.e., it comes from another disease that worsens bone quality? For example, from an overactive thyroid, an inflammatory disease such as rheumatoid arthritis or Crohn’s disease, or Renal osteopathy, in which chronic renal insufficiency disrupts mineral metabolism? Then, the first thing to do is tackle these underlying diseases. It remains to be seen whether natural and empirical medicine is worse at this than conventional medicine.
Which drugs damage our bones
Drugs urgently need to be examined. Antidepressants, particularly the so-called selective serotonin reuptake inhibitors (SSRIs), reduce bone density; in a US study, the risk of bone fractures was 76% higher after just one year of use than in a control group without SSRIs.
Gastric acid blockers – proton pump inhibitors – such as Prilosec also damage our skeleton. Steroids such as prednisone also significantly increase the risk of osteoporosis; in typical doses, they cause an annual bone loss of 5 to 15%. The risk of bone fractures, particularly in vertebrae, doubles; in patients who take high doses of steroids, it even increases fivefold. 37% of all long-term users will suffer from vertebral fractures at some point.
Certain drugs for type 2 diabetes, known as glitazones, also increase the risk of bone fractures after menopause – it doubles. This is particularly fatal for diabetics because hip fractures are already twice as common among them.
Hormone blockers such as Lupron, which switch off the body’s own production of sex hormones, are extremely dangerous. They weaken the skeleton so much that some sufferers complain that they have “bones like an 80-year-old”. An American doctor reports cases of young adults whose arm bones broke when they leaned against a house wall or were told by their dentist that they needed dentures.
Aromatase inhibitors are also a cause for concern. They reduce estrogen production in the body by blocking an enzyme that helps convert male hormones (such as testosterone) into female ones. This can also trigger bone loss.
“The truth is simple.”
Why do you think there are significantly fewer osteoporotic hip fractures per 100,000 inhabitants in West Africa (3) than in Europe (408 in Austria, 532 in Norway)?
“The truth is simple,” Buddha taught – so simple that even the unfortunate Ottilie could have understood it. The most important thing to note about the prevention and treatment of osteoporosis does not require a thick textbook – it fits into a single line: Get plenty of exercise in the fresh air. And eat healthily for the rest of your life.
Medicine could sometimes be that simple. But there would simply be nothing more to be earned from such a practice for the medical-industrial complex.
(Harald Wiesendanger)
Notes
1 WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland) (2003). “Prevention and management of osteoporosis: report of a WHO scientific group” (PDF)
2 WHO (1994) “Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group“. World Health Organization technical report series 843: 1-129
3 “Kaukasier” –engl. caucasian – ist ein in medizinischen Publikationen nach wie vor gängiger Begriff. Er umfasst, wissenschaftlich verbrämt, nichts anderes als Menschen mit heller Haut: fast alle Europäer und westliche Asiaten. Den Terminus prägte der deutsche Anthropologe Johann Friedrich Blumenbach (1752-1840) vor über 200 Jahren.
4 Zit. nach Gina Kolata: “Bone Diagnosis Gives New Data But No Answers“, New York Times, 28.9.2003
5 Prävalenz und Inzidenz der Osteoporose und ihrer Folgen, sozioökonomische Relevanz | DVO Leitlinie Osteoporose 2023
6 http://www.ncbi.nlm.nih.gov/pubmed/9663400; https://pubmed.ncbi.nlm.nih.gov/11416114/; https://pubmed.ncbi.nlm.nih.gov/15469036/
7 https://www.bmj.com/content/341/bmj.c3691.full; https://pubmed.ncbi.nlm.nih.gov/21505219/
8 https://acteurdemasante.lu/de/rheumatologie/osteoporose-behandlung-hormontherapie-und-verwandte-behandlungsmethoden/; https://wechseljahre-verstehen.de/hormonersatztherapie/praeventiver-zusatznutzen-einer-hrt/; https://www.hormonspezialisten.de/indikationen/wechseljahresbeschwerden/osteoporose/
9 https://www.frauenaerzte-im-netz.de/koerper-sexualitaet/wechseljahre-klimakterium/hormonersatztherapie-hrt/; https://www.aok.de/pk/magazin/koerper-psyche/organe/hormonersatztherapie-wirkung-und-risiken/; https://www.hormonspezialisten.de/indikationen/wechseljahresbeschwerden/hrt-nutzen-risiko/; www.ncbi.nlm.nih.gov/pubmed/18319414
10 https://en.wikipedia.org/wiki/Selective_estrogen_receptor_modulator; https://flexikon.doccheck.com/de/Selektiver_Estrogenrezeptormodulator; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4995266/
11 https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00325/full; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924518/; https://arthritis-research.biomedcentral.com/articles/10.1186/ar2167
12 https://flexikon.doccheck.com/de/Denosumab; https://www.gelbe-liste.de/wirkstoffe/Raloxifen_44775; https://www.pharmazeutische-zeitung.de/vielfalt-in-einer-stoffklasse/
13 https://www.fortunebusinessinsights.com/de/industrie-berichte/osteoporose-behandlungsmarkt-101034; https://www.gminsights.com/de/industry-analysis/postmenopausal-osteoporosis-treatment-market
14 So heißt es nach dem Berliner Anatom und Chirurgen Julius Wolff. Es besagt: Der Knochen passt sich in seiner Form und Struktur an die auf ihn einwirkenden mechanischen Belastungen an. Reichen sie aus, so baut sich der Knochen auf und nimmt an Festigkeit und Knochendichte zu. Bei fehlender oder geringer Belastung hingegen baut er sich ab. Siehe https://de.wikipedia.org/wiki/Wolffsches_Gesetz; https://www.osd-ev.org/osteoporose/knochen/belastung/; https://jwi.charite.de/publikationen/julius_wolff_buch/
15 https://onlinelibrary.wiley.com/doi/10.1002/jbmr.3070; https://www.health.harvard.edu/newsletter_article/anti-inflammatory-diet-could-reduce-risk-of-bone-loss-in-women
16 Über 85% des Phosphors in unserem Körper befinden sich in anorganischen Verbindungen mit Calcium, hauptsächlich im Skelett und in den Zähnen: https://www.vitalstoff-lexikon.de/Mineralstoffe/Phosphor/Definition-Synthese-Resorption-Transport-und-Verteilung; https://www.eucell.de/ernaehrung/ernaehrungslexikon/mineralstoffe/phosphor
17 https://www.rosenfluh.ch/media/ernaehrungsmedizin/2011/01/08_Silizium_1.11.pdf; https://www.gesundheitswissen.de/gesund-leben/behandlung-therapie/vorsorge/weiche-knochen-ade-schuetzen-sie-sich-mit-silizium-vor-osteoporose/
18 https://pubmed.ncbi.nlm.nih.gov/12700617/; https://www.rosenfluh.ch/media/ernaehrungsmedizin/2011/02/08_Mikronaehrstoffe_2.11.pdf
19 https://air.unimi.it/retrieve/ec230269-9f1c-45a2-8c9a-7c2a73956765/Rondanelli%20M%20-%20J%20Trace%20Elem%20Med%20Biol%202020.pdf; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4712861/ https://www.rosenfluh.ch/media/ernaehrungsmedizin/2011/02/08_Mikronaehrstoffe_2.11.pdf
20 https://www.zentrum-der-gesundheit.de/bibliothek/sonstige-informationen/weitere-informationen/heilpflanzen-starke-knochen-ia; https://www.naturheilt.com/osteoporose/